A nurse is teaching a client how to self-administer insulin, a critical aspect of diabetes management. This educational process involves effective communication, fostering a supportive learning environment, and ensuring the client’s understanding of insulin administration techniques, monitoring, and lifestyle management.
Through this collaboration, the nurse empowers the client to self-manage their diabetes, promoting adherence to treatment plans and overall well-being.
Nurse-Client Interaction
Nurses play a pivotal role in educating clients on self-insulin administration. Effective communication and patient understanding are paramount. Nurses must foster a supportive learning environment, utilizing strategies such as active listening, empathy, and providing clear instructions.
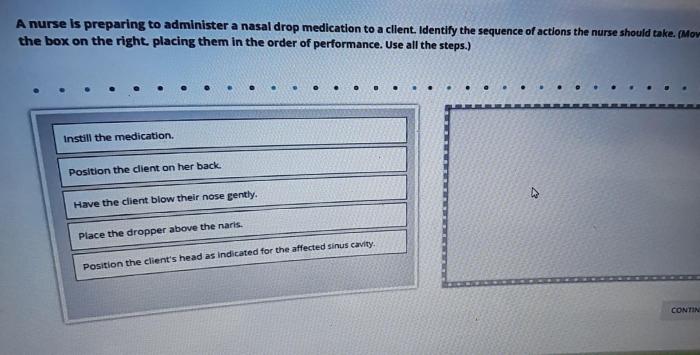
Insulin Administration Techniques
Insulin administration involves preparing and injecting insulin using devices like pens or syringes. Factors influencing dosage and timing include blood glucose levels, diet, and activity. The table below summarizes different insulin types and their onset and duration of action:
| Insulin Type | Onset | Duration |
|---|---|---|
| Rapid-acting | 15-30 minutes | 3-5 hours |
| Short-acting | 30-60 minutes | 6-8 hours |
| Intermediate-acting | 1-2 hours | 12-18 hours |
| Long-acting | 2-4 hours | 24 hours or more |
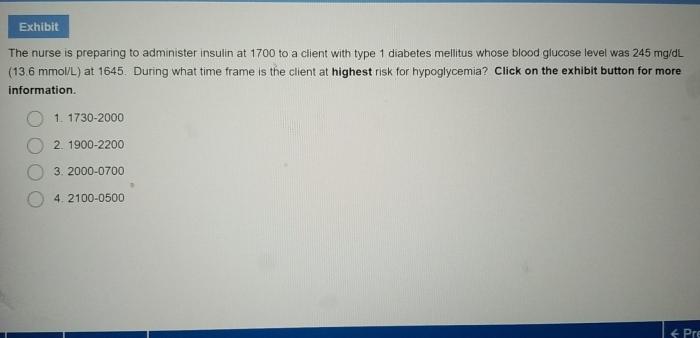
Monitoring and Troubleshooting
Regular blood glucose monitoring is essential. Signs and symptoms of hypoglycemia include shakiness, sweating, and confusion. Hyperglycemia symptoms include thirst, frequent urination, and fatigue. Insulin doses should be adjusted based on blood glucose readings. Common challenges include injection site reactions and insulin resistance.
Lifestyle Management

Diet, exercise, and stress management impact blood glucose control. Healthy eating habits include fruits, vegetables, and whole grains. Regular physical activity improves insulin sensitivity. Stress management techniques like yoga or meditation can reduce blood glucose levels.
Patient Empowerment: A Nurse Is Teaching A Client How To Self-administer Insulin
Nurses empower clients to self-manage diabetes. Strategies include setting realistic goals, providing ongoing support, and promoting self-efficacy. Resources and support systems for clients with diabetes include diabetes education programs, support groups, and online forums.
Q&A
What is the nurse’s primary role in teaching insulin self-administration?
The nurse’s primary role is to educate the client on proper insulin preparation, injection techniques, monitoring, and lifestyle management to ensure safe and effective self-administration.
Why is effective communication crucial in this educational process?
Effective communication allows the nurse to assess the client’s understanding, address any misconceptions, and tailor the education to meet the client’s individual needs and learning style.
How does the nurse foster a positive learning environment?
The nurse creates a supportive and non-judgmental environment by actively listening, using clear and simple language, and encouraging questions and feedback from the client.